Many people underestimate the significance of fat tissue beyond mere weight gain, as dysfunctional fat can lead to serious health issues like metabolic syndrome. Understanding how to assess your fat tissue’s function can provide vital insights into your metabolic health. By utilizing specific measurements and monitoring key biomarkers, you can identify risks early. So, what steps can you take to evaluate your fat tissue effectively and proactively manage your health?
Key Takeaways
- Measure waist circumference regularly; values over 40 inches for men and 35 inches for women indicate increased visceral fat risk for metabolic syndrome.
- Utilize Body Mass Index (BMI) alongside waist measurements to assess overall body composition, while being mindful of its limitations.
- Conduct skinfold measurements with a trained professional to evaluate subcutaneous fat and monitor changes over time.
- Perform blood tests to evaluate key biomarkers like glucose, insulin, and triglycerides, which indicate insulin resistance and metabolic health.
- Consider bioelectrical impedance analysis (BIA) for a quick, non-invasive estimate of body fat percentage, helping to identify early signs of dysfunctional fat tissue.
Understanding Dysfunctional Fat Tissue
Understanding dysfunctional fat tissue is vital because it plays a significant role in various metabolic disorders. This tissue isn’t merely an energy reservoir; it actively secretes hormones and cytokines that influence insulin sensitivity and inflammation.
Dysfunctional fat tissue influences metabolic health by secreting hormones that affect insulin sensitivity and inflammation.
When fat tissue becomes dysfunctional, often characterized by hypertrophy and inflammation, it disrupts metabolic homeostasis. You might observe increased levels of free fatty acids and inflammatory markers, which can lead to insulin resistance.
Research indicates that dysfunctional adipocytes can contribute to a pro-inflammatory state, exacerbating conditions like type 2 diabetes. By recognizing these characteristics, you can better evaluate your own metabolic health.
Analyzing fat distribution and cellular function is important for early intervention, allowing you to mitigate the risks associated with metabolic dysregulation before they escalate.
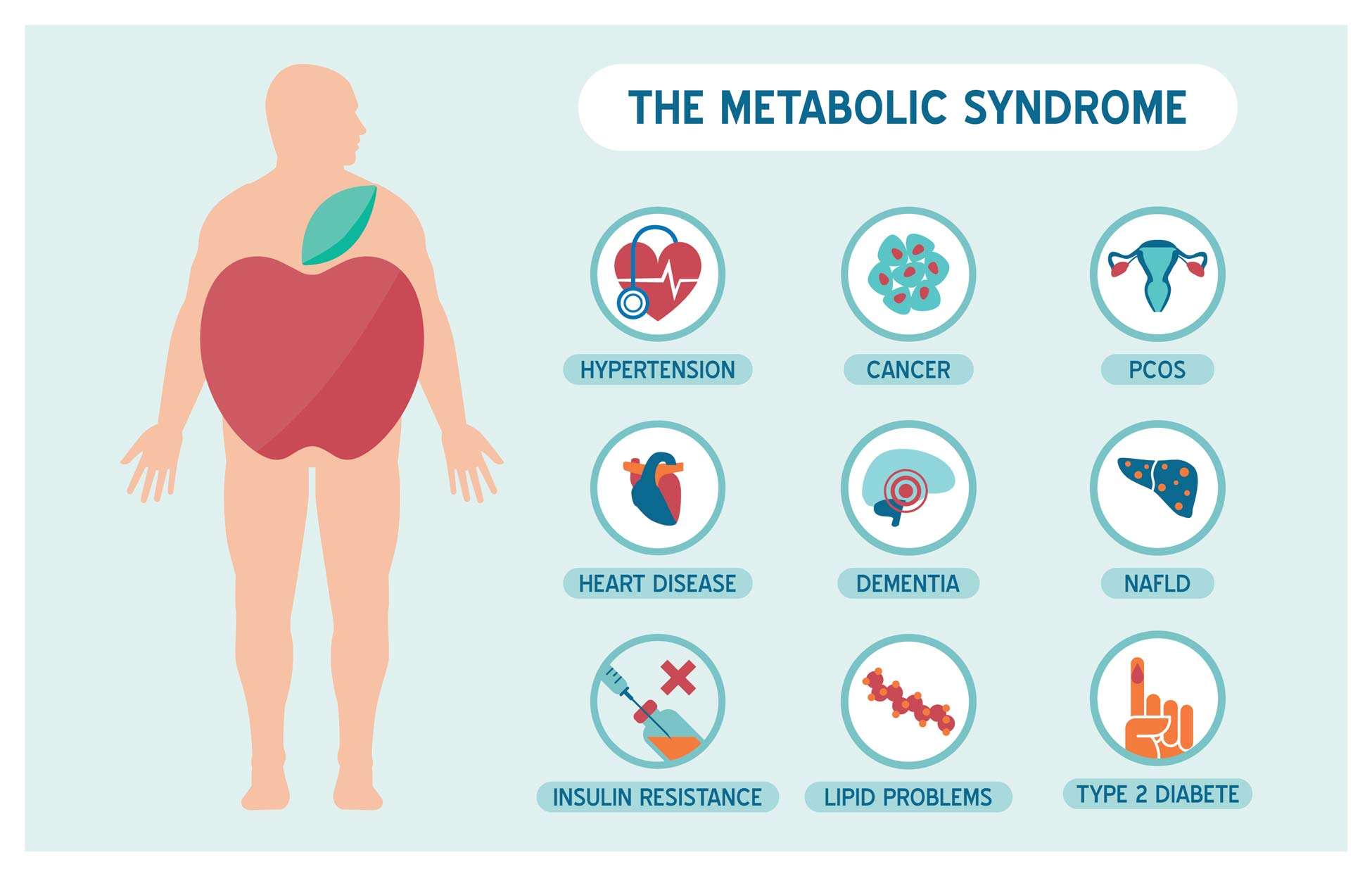
The Role of Metabolic Syndrome
Dysfunctional fat tissue is closely linked to metabolic syndrome, a cluster of conditions that greatly increases the risk of heart disease, stroke, and type 2 diabetes. Metabolic syndrome often manifests through insulin resistance, hypertension, and dyslipidemia. Understanding how these elements interact can help you in early identification and intervention.
| Condition | Description | Impact on Health |
|---|---|---|
| Insulin Resistance | Decreased ability to respond to insulin | Elevated blood glucose levels |
| Hypertension | High blood pressure | Strain on cardiovascular system |
| Dyslipidemia | Abnormal lipid levels | Increased atherosclerosis risk |
| Abdominal Obesity | Excess fat in the abdominal area | Inflammation and hormonal imbalance |
| Inactivity | Sedentary lifestyle | Exacerbates all conditions |
Recognizing these factors is essential for preventing the progression of metabolic syndrome.
Identifying Risk Factors
When considering dysfunctional fat tissue, it’s vital to identify the risk factors that contribute to its development.
Genetic predisposition plays a significant role, as certain genes can increase your susceptibility to metabolic disorders.
Additionally, lifestyle influences, such as diet and physical activity, can further exacerbate these risks, making it essential to analyze both aspects for effective prevention and intervention strategies.
Genetic Predisposition Factors
Genetic predisposition plays an essential role in determining an individual’s risk for developing dysfunctional fat tissue. Understanding these factors can help you assess your vulnerability to metabolic syndrome.
Here are key genetic aspects to contemplate:
- Family History: A background of obesity or metabolic disorders in your family can increase your risk.
- Specific Genes: Variants in genes like FTO and MC4R are linked to body fat distribution.
- Ethnic Background: Certain ethnic groups exhibit higher genetic risks for fat dysfunction.
- Hormonal Regulation: Genetic factors affect hormone levels that regulate appetite and fat storage.
- Age-Related Changes: Genomic changes over time can influence your fat distribution and metabolism.
Lifestyle Influences Analysis
Although genetic factors contribute considerably to the risk of dysfunctional fat tissue, lifestyle choices play an equally critical role in shaping your metabolic health. Your dietary habits, physical activity levels, and stress management practices directly influence fat distribution and functionality.
High sugar and saturated fat consumption can lead to insulin resistance, exacerbating the risk for metabolic syndrome. Conversely, a balanced diet rich in fiber, lean proteins, and healthy fats supports optimal metabolic function. Regular exercise enhances insulin sensitivity and promotes healthy fat metabolism.
Additionally, chronic stress elevates cortisol levels, which can lead to fat accumulation, particularly in the abdominal area. By addressing these lifestyle factors, you can greatly reduce your risk of developing dysfunctional fat tissue and metabolic disorders.
Body Mass Index (BMI) Assessment
When evaluating body composition, it’s essential to recognize the limitations of Body Mass Index (BMI) as a sole indicator of health.
While BMI provides a quick measurement of weight relative to height, it often overlooks factors like muscle mass and fat distribution.
Exploring alternative assessment methods can offer a more thorough understanding of an individual’s health status.
Understanding BMI Limitations
While BMI serves as a convenient tool for evaluating body weight relative to height, it has significant limitations that can obscure an accurate understanding of an individual’s health.
Relying solely on BMI can lead to misconceptions about health risks associated with body composition.
- It doesn’t differentiate between muscle and fat mass.
- It overlooks fat distribution, a critical factor in metabolic health.
- It fails to account for variations across different ethnicities.
- It can misclassify athletes as overweight or obese.
- It doesn’t consider age-related changes in body composition.
These limitations underscore the importance of a thorough assessment.
Understanding these flaws can guide you toward more effective strategies for evaluating overall health and addressing potential metabolic issues before they escalate.
Alternative Assessment Methods
Exploring alternative assessment methods can provide a more nuanced view of your health beyond what BMI offers. Techniques like body composition analysis, which measures fat versus lean mass, can reveal insights into your metabolic health.
Waist circumference and waist-to-hip ratio assessments can indicate visceral fat levels, a key factor linked to metabolic syndrome. Additionally, advanced imaging modalities, such as MRI or CT scans, can provide detailed depictions of adipose tissue distribution and functionality.
These methods can help you understand the quality of fat tissue, rather than just quantity. Integrating these assessments can empower you to tailor lifestyle changes, monitor progress more effectively, and ultimately reduce the risk of developing metabolic syndrome.
Waist Circumference Measurement
Waist circumference measurement serves as a vital indicator of abdominal fat and overall health. This simple assessment can provide significant insights into your metabolic risk factors.
Here are key points to reflect on:
- It reflects visceral fat accumulation, which is linked to metabolic syndrome.
- Measurement should be taken at the narrowest part of your waist, ideally in a standing position.
- For men, a circumference of over 40 inches is concerning; for women, over 35 inches is alarming.
- Regular monitoring can help track changes in fat distribution over time.
- This method is cost-effective and requires minimal training, making it accessible for widespread use.
Skinfold Thickness Testing
Following waist circumference measurement, skinfold thickness testing offers another effective method to assess body fat composition. This technique involves measuring the thickness of skinfolds at specific sites on your body, typically using calipers.
By targeting areas like the triceps, abdomen, and thigh, you can estimate subcutaneous fat levels, which correlate with overall body fat percentage. Research supports the reliability of skinfold measurements when performed consistently by trained professionals.
However, accuracy can diminish if techniques vary. It’s essential to maintain a standardized approach, including proper site selection and caliper pressure.
Bioelectrical Impedance Analysis
While skinfold thickness testing provides valuable insights, bioelectrical impedance analysis (BIA) offers a different approach to evaluating body fat composition. This method utilizes electrical currents to estimate body fat percentage and distribution, making it a non-invasive and efficient option.
- Quick results: BIA can deliver measurements in a matter of minutes.
- Hydration status: It accounts for fluid levels, which can affect accuracy.
- Accessibility: BIA devices are widely available and user-friendly.
- Reproducibility: Regular use can track changes over time reliably.
- Cost-effective: It’s often more affordable than other body composition methods.
Dual-Energy X-ray Absorptiometry (DEXA)
When you’re looking for a highly accurate method to assess body composition, Dual-Energy X-ray Absorptiometry (DEXA) stands out as a leading choice.
This technique uses low-dose X-ray beams to differentiate between bone mass, lean tissue, and fat tissue. DEXA provides precise measurements of fat distribution, allowing you to identify visceral fat, which is closely linked to metabolic syndrome.
DEXA utilizes low-dose X-ray beams to accurately measure bone, lean, and fat tissue, revealing crucial insights into visceral fat and metabolic health.
The high-resolution images generated enable you to evaluate regional fat deposits, offering insights into potential health risks. Unlike other methods, DEXA’s reproducibility and reliability make it the gold standard in body composition analysis.
Regular assessments can help you monitor changes over time, providing critical data for tailoring lifestyle interventions aimed at preventing metabolic dysfunction.
Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) offers a non-invasive method to visualize fat distribution in the body, providing insights into its role in metabolic health.
MRI Technology Overview
MRI technology, a cornerstone of modern medical imaging, employs powerful magnetic fields and radio waves to generate detailed images of the body’s internal structures. This non-invasive technique is invaluable for analyzing fat distribution and identifying potential dysfunctions in adipose tissue.
- High-resolution imaging allows for precise evaluation of tissue characteristics.
- MRI can differentiate between subcutaneous and visceral fat.
- It provides critical insights without exposing patients to ionizing radiation.
- This technology can track changes in fat composition over time.
- MRI is effective for studying metabolic disorders and their impact on health.
Identifying Fat Distribution
Understanding fat distribution is essential for evaluating health risks associated with obesity and metabolic disorders. Magnetic Resonance Imaging (MRI) provides precise insights into how fat is distributed in your body, allowing for a better understanding of potential health issues.
| Fat Type | Distribution Area | Health Implications |
|---|---|---|
| Subcutaneous | Beneath the skin | Generally less harmful |
| Visceral | Surrounding organs | Increased risk for disease |
| Ectopic | Muscle and liver | Linked to metabolic dysfunction |
Assessing Metabolic Health Risks
Evaluating metabolic health risks requires an all-encompassing approach that goes beyond merely identifying fat distribution.
Magnetic Resonance Imaging (MRI) serves as a powerful tool in this assessment, providing detailed insights into fat composition and distribution at a cellular level.
Consider these key aspects of MRI in evaluating metabolic health:
- Accurate visualization of visceral vs. subcutaneous fat
- Identification of ectopic fat in organs like the liver and pancreas
- Assessment of fat quality, distinguishing between healthy and dysfunctional adipose tissue
- Non-invasive method with no radiation exposure
- Ability to track changes in fat distribution over time
Blood Tests for Metabolic Health
As scientists uncover the complexities of metabolic health, blood tests have emerged as crucial tools for evaluating the function of fat tissue and its broader implications on overall well-being.
These tests can measure key biomarkers such as glucose, insulin, triglycerides, and cholesterol levels, providing insights into your metabolic state. Elevated insulin and triglyceride levels, for instance, often indicate insulin resistance, a precursor to metabolic syndrome.
Additionally, analyzing lipid profiles can reveal dyslipidemia, which is linked to cardiovascular risk. Regular blood testing allows you to monitor these indicators over time, enabling early intervention and lifestyle adjustments.
Identifying Inflammation Markers
To understand the relationship between dysfunctional fat tissue and inflammation, you need to identify key inflammatory biomarkers present in your blood.
These markers can provide insights into your metabolic health and help assess the impact of your lifestyle choices.
Key Inflammatory Biomarkers
Identifying key inflammatory biomarkers is essential for understanding the role of dysfunctional fat tissue in metabolic diseases.
These biomarkers provide insight into the inflammatory processes that contribute to metabolic syndrome. By monitoring these indicators, you can track the progression of dysfunction and adjust interventions accordingly.
- C-reactive protein (CRP): A marker of systemic inflammation.
- Interleukin-6 (IL-6): Involved in inflammatory responses and metabolic regulation.
- Tumor necrosis factor-alpha (TNF-α): Key player in obesity-related inflammation.
- Adiponectin: An adipokine with anti-inflammatory properties, inversely related to fat mass.
- Fibrinogen: A coagulation factor that can reflect chronic inflammation levels.
Understanding these biomarkers will empower you to make informed decisions regarding your health.
Blood Tests Overview
Understanding the nuances of blood tests is essential when evaluating inflammation markers linked to dysfunctional fat tissue. Key markers such as C-reactive protein (CRP) and interleukin-6 (IL-6) provide insights into systemic inflammation. Elevated CRP levels indicate an inflammatory response, while IL-6 plays a significant role in regulating metabolic processes.
Additionally, measuring adipokines like leptin and adiponectin can reveal the functional status of adipose tissue. High leptin and low adiponectin levels are often associated with inflammation and metabolic dysregulation.
Regularly monitoring these biomarkers allows for early identification of potential issues, enabling targeted interventions. By understanding these tests, you can effectively track your metabolic health and address concerns before they escalate into metabolic syndrome.
Lifestyle Impact Assessment
Monitoring lifestyle factors is essential for evaluating inflammation markers that indicate dysfunctional fat tissue. By understanding how your habits influence inflammation, you can proactively address potential health risks.
Consider these critical aspects:
- Diet Quality: Assess your intake of processed foods and sugars.
- Physical Activity: Track the frequency and intensity of your exercise routines.
- Sleep Patterns: Evaluate the quality and duration of your sleep.
- Stress Levels: Identify stressors and their impacts on your overall well-being.
- Alcohol Consumption: Monitor your intake and its effects on metabolic health.
Each of these elements can contribute to inflammation levels, affecting your risk of developing metabolic syndrome.
Monitoring Blood Pressure
How do you guarantee that your blood pressure remains within a healthy range? Regular monitoring is essential. Aim for at least weekly checks, utilizing a reliable sphygmomanometer. Target a systolic reading below 120 mmHg and diastolic below 80 mmHg. Elevated readings may indicate developing dysfunction in fat tissue, linking to metabolic syndrome.
Additionally, consider factors influencing blood pressure: diet, stress, and sleep quality. A diet rich in potassium, magnesium, and omega-3 fatty acids can promote vascular health. Reducing sodium intake is also vital.
Engage in regular relaxation techniques to mitigate stress. If readings consistently exceed recommended levels, consult a healthcare professional for tailored strategies. Monitoring your blood pressure empowers you to take proactive steps in maintaining your metabolic health.
Tracking Physical Activity Levels
Are you aware of how your physical activity levels affect your metabolic health? Tracking your activity can provide insights into how your body manages fat storage and insulin sensitivity.
Here are some key aspects to evaluate:
- Frequency: Regular activity can enhance metabolic flexibility.
- Duration: Longer sessions of moderate exercise can improve fat oxidation.
- Intensity: High-intensity workouts may optimize hormonal responses.
- Type: Resistance training can increase muscle mass, boosting metabolism.
- Consistency: Adhering to a routine fosters long-term metabolic benefits.
Making Lifestyle Changes for Prevention
While many people focus on immediate results, making lifestyle changes aimed at prevention can greatly enhance long-term metabolic health. Incorporating a balanced diet rich in whole foods—fruits, vegetables, lean proteins, and healthy fats—fuels metabolic efficiency and reduces the risk of dysfunctional fat accumulation.
Regular aerobic and resistance training not only enhances physical fitness but also improves insulin sensitivity, a key factor in preventing metabolic syndrome. Prioritizing sleep hygiene and managing stress through mindfulness techniques can further support hormonal balance, which is vital for maintaining healthy fat tissue.
Final Thought
In the battle against metabolic syndrome, recognizing dysfunctional fat tissue is essential. By measuring waist circumference and evaluating body fat percentage, you can uncover hidden risks. While a healthy BMI offers a glimpse of wellness, it’s the details—like inflammation markers and blood pressure—that reveal deeper truths. Embracing lifestyle changes can transform potential threats into opportunities for well-being. Ultimately, proactive monitoring and mindful choices empower you to reclaim your health before complications arise, turning uncertainty into strength.
Post Disclaimer
This post is based on research and expert insights, reviewed by healthcare professionals for accuracy. It is for informational purposes only and not a substitute for professional medical advice. Always consult a qualified healthcare provider before making health-related decisions.